Are all GABAA receptor variant seizures due to reduced efficacy of GABA receptor signaling?
The consensus to date suggests that reduced efficacy of GABAergic inhibition leads to developmental and epileptic encephalopathy. This is plausible given the key role of GABAergic inhibition in controlling neural excitability. However, our recent work suggests that gain-of-function variants of GABAA receptors can also underlie seizures.
In this study, while characterising GABAA receptor variants of a predominant receptor subtype, we discovered that spontaneous GABAA receptor mutations can counterintuitively underlie seizures. We were able to reverse some of the phenotypic anomalies by using a naturally produced inhibitory neurosteroid with important implications for therapy of this emerging class of genetic epilepsies.
The approach
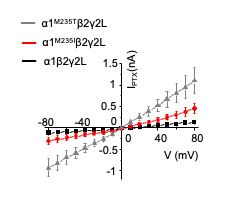
Using whole cell patch clamp recordings, we found two GABAA receptor α1 subunit first transmembrane domain variants M263K (M235K without signal sequence) and L267I (L239I without signal sequence) are spontaneously active, revealed by the application of the open channel blocker picrotoxin.
We also found that this key region in the first transmembrane domain which forms an integral endogenous neurosteroid binding site is a hot-spot for spontaneously active GABAA receptor developmental and epileptic encephalopathy variants (see below)

Large tonic GABAA receptor conductances due to spontaneously active variants
Expression of M263K (M235K without signal sequence) and L267I (L239I without signal sequence) in hippocampal neurons resulted in extraordinarily high tonic GABA currents which were revealed by application of the GABAA receptor antagonist bicuculline.
In addition, application of the open channel blocker picrotoxin in the presence of bicuculline revealed a second spontaneous tonic current in variants that was absent in wild-type neurons.

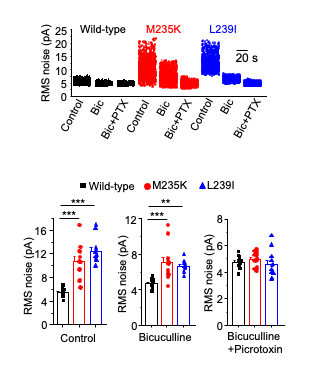
Large membrane noise due to spontaneously active variants
Expression of M263K (M235K without signal sequence) and L267I (L239I without signal sequence) in hippocampal neurons resulted in high membrane noise revealed by application of the GABAA receptor antagonist bicuculline.
In addition, application of the open channel blocker picrotoxin revealed a second spontaneous noise component in variants that was absent in wild-type neurons.
Altered structural plasticity of dendritic spines due to spontaneously active variants
Expression of M263K (M235K without signal sequence) and L267I (L239I without signal sequence) in hippocampal neurons resulted in reduced dendritic spine density and percentage of mature or mushroom spines with a concomitant increase of percentage of thin or immature spines.

An inhibitory neurosteroid reverses deficits in dendritic spine plasticity
Application of a naturally occurring, inhibitory neurosteroid pregnenolone sulphate normalised dendritic spine defects for L239I. For M235K, spine density showed a tendency to increase in pregnenolone sulphate compared to untreated M253K-expressing cells.

A hot-spot for spontaneously active GABAA receptor variants
We studied two additional variants at the first transmembrane domain M235 site that are linked to West syndrome severe epilepsy and intellectual disability.
These variants (human M263I and M263T, numbered by including the signal sequence and equivalent to mouse M235I and M235T in the mature protein) also showed spontaneity, revealed by picrotoxin, suggesting that the transmembrane methionine residue is crucial for GABAA receptor function.
For more details please visit the publication:
*corresponding authors